The Faculty of Health has a long history of partnering with industry and community in education and research. This is a major feature of Associate Professor Jo River’s research, which centres community and industry knowledge using methods such as co-design, co-production and deliberative dialogue. More recently, River decided to take their educational design to the next level by partnering with community members and clinical experts to design and deliver postgraduate mental health curricula.
The growing emphasis on embedding industry and community perspectives in healthcare curricula ensures that our educational offerings are meeting community and industry expectations. It can also prepare students for practice, ensuring that they have the required knowledge and skills to offer care in contemporary health services.
Defining co-design and collaboration
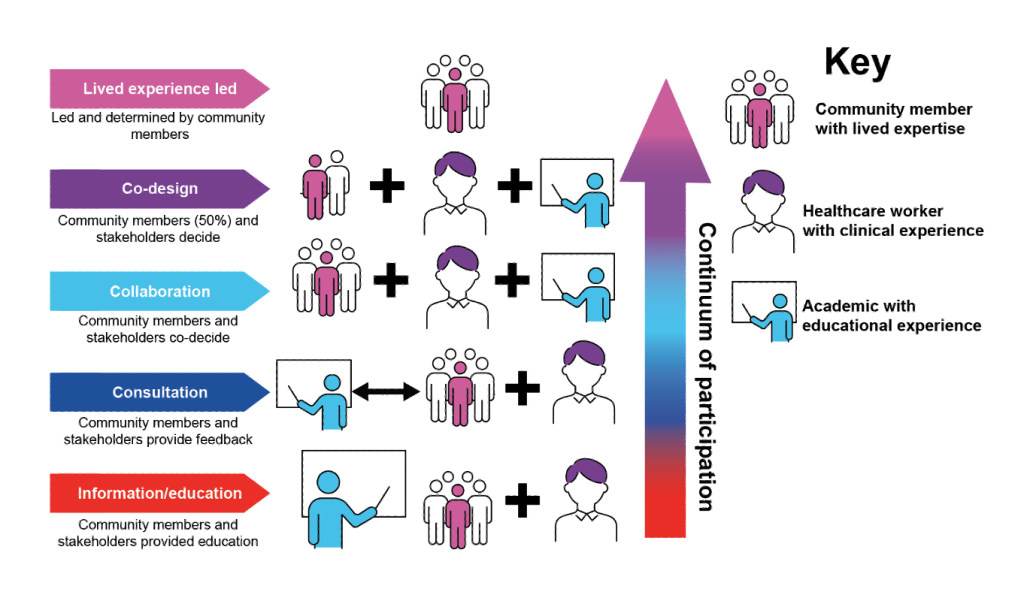
Involvement sits on a continuum. Many are familiar with consultation as inviting community members with lived experience and clinicians to provide feedback on education offering – but higher levels of participation are possible, and include collaborative design and co-design approaches.
Early on in the process of designing an OPM subject, the team determined that, for design to be considered ‘co-design’, they required 50% or more of the team to be community members with lived experience, and that community members, clinicians, and academics would have equitable decision-making power across all stages of design and delivery of curriculum. We used the term ‘collaboration’ when we had an equitable decision-making process and partnership in all stages of design and delivery, but community members made up less than 50% of the team.
Designing with industry and community experts
Prior to commencing the design process, River consulted broadly to get an understanding of community expectations and industry perspectives on a topic. They also undertook a desktop review of relevant research.
Then, they brought together a team of clinicians, academics and community members with a lived experience to partner through all stages of the design. These stages include deciding the key learning objectives and outcomes, designing the content and assessments, and co-delivering the subject.
It was about working it out together, drawing on consultation information, the evidence and the team’s diverse expertise (lived/clinical/educational/research) to create the best educational offering possible. One that meets the needs of the people with lived experience, of health services and of our students.
To ensure that the process doesn’t fall back to being consultation, the collaborative or co-design team agreed on clear objectives, hold regular meetings and have a clear decision-making process. They also checked in regularly to ensure that everyone was happy with where the design is going. The collaborative teams then worked with the Learning Design Team to bring the ideas to life.
Inclusive learning design through lived experiences and illustrations – by Glendon Gardner and Amelia Di Paolo
A key focus during the design process was making sure that people with lived experience of mental health challengeswere represented in a respectful and inclusive way. We wanted to share their stories honestly, while avoiding negative stereotypes that can reinforce stigma.
The design team used hand-drawn line illustrations to represent everyday people of different ethnicities, genders, body types, and backgrounds. This helps communicate that mental health challenges can affect anyone and aims to reduce assumptions, supporting a shared sense of humanity.
A/Prof River and team, in collaboration with the Educational Media Team, also co-designed a video explaining the idea of multiple explanatory frames for mental distress. In this case, the Educational Media Team used silhouettes rather than detailed images, to reflect people’s identities through their stories.
Bridging the gap between theory and practice
The collaboratively designed subjects have been well received, with high student satisfaction scores, and one student remarking that it was highly relevant and informative for their practice, and one of the “most valuable and interesting courses I’ve taken at UTS”.
Co-teaching with people with lived experience and clinical experts can also shift student perspectives and help to bridge the gap between theory and practice. For example, when we’re teaching about collaboration, the students can see the team embodying and practising it as they teach together. Students also get to ask about the challenges and difficulties of working in this way from people they trust are actually doing it, and get to hear perspectives from our different positions as community members, clinicians or educators.
The design teams are now planning to consult with past students and bring them into the design team to refine the educational offers to ensure they meet students’ diverse learning needs. If you want to read more about the co-designed and collaboratively designed subjects in the OPM program, you can read about them here.
