A/Prof. Ken Rodgers School of Life Sciences

Learning Objectives
- Recognise health care costs associated with Adverse Drug Reactions (ADRs)
- Outline the contribution of the following to the overall burden of preventable ADRs
- Age
- Pharmacogenetics
- Diseases
- Idiosyncratic reactions
- Drug interactions
- Identify mechanisms for specific clinically relevant drug interactions
- Identify issues of polypharmacy in the elderly
- Provide approaches to minimise ADRs
References
- Rang and Dales Pharmacology (8th ed)
- Chapters 11 and 57. Individual Variation and Drug Interactions. Harmful effects of drugs
- World Health Organisation
- The Food and Drug Administration (FDA) Center for Drug Evaluation and Research
- Therapeutic Goods Administration (TGA)
Intro to Drug Interactions

Drug Interactions
- A drug interaction is said to occur when the effects of one drug are changed by the presence of another drug, food, drink or by some environmental chemical
- Drug-Drug Interaction
- Occurs when effects of one drug are increased or decreased by previous or concurrent administration of another drug

Drug Interactions: Introduction
- Contribution of Drug Interactions to the Overall Burden of Preventable ADRs
- Drug interactions represent 3–5% of preventable in-hospital ADRs
- Drug interactions are an important contributor to number of ER visits and hospital admissions

Drug Interactions: Introduction
- The administration of one drug (A) can alter the action of another (B) by:
- Modification of the pharmacological effect of B without altering its conc (pharmacodynamic interaction)
- Alteration of the conc of B that reaches its site of action (pharmacokinetic interaction)
- >6 medications = >80% chance of interaction
- Consequence: alter dose / change medication
Drug Interactions: Introduction
- For pharmacokinetic interactions to be clinically important, it is also necessary that the dose-response curve is steep
- A small reduction in plasma conc will lead to a substantial change in effect
- For most drugs these conditions are not met since therapeutic margin is usually large (eg penicillin >100)

Repeated doses 2


Drug Interactions: Introduction
- Several drugs have a steep dose-response relationships and a narrow therapeutic margin
- Drug interactions can cause major problems with these drugs
- Antithrombotic drugs
- Antiarrhythmic drugs
- Antiepileptic drugs
- Lithium
- Several antineoplastic drugs
- Several immunosuppressant drugs
Drug Interactions: Pharmacodynamic
Pharmacodynamic
- Often predictable from the actions of the interacting drugs
- Additive
- Nephrotoxicity – cyclosporin and aminoglycosides
- Sedation – H1 receptor antagonists and alcohol
- Synergistic (different mechanisms of action)
- Bleeding risk – aspirin and warfarin
- Rx of Pneumocystis carinii – sulfonamides and trimethoprim
- Antagonistic
- Reduction of antihypertensive action – NSAIDsand diuretics
- Bronchoconstriction – β-blockers and salbutamol
- Block of coagulation – warfarin and vitamin K-containing foods
- Beta2-adrenoceptor antagonist + agonist
Drug Interactions: Pharmacokinetic
- 2. Pharmacokinetic
- Absorption of the drug into systemic circulation
- Distribution of the drug to the site of action and into tissues
- Metabolism of the drug to polar intermediates
- Elimination of the drug from the body
Absorption
Drug Interactions: Absorption
Absorption in the GI Tract


Drug Interactions: Absorption
- Absorption (non-GIT)
- Prevented by complex formation with others substances
- Phenytoin precipitates in dextrose solutions (e.g. D5W)
- Amphotericin precipitates in saline
- Prevented by complex formation with others drugs
- Thiopentone and suxamethonium shouldn’t be mixed in same syringe
- Gentamicin complexes with beta-lactams and certain plastics – loss of antibiotic effect
- Slowed by drugs that cause vasoconstriction at injection site
- Adrenaline and local anaesthetics
- Prevented by complex formation with others substances
Distribution

Drug Interactions: Distribution
- Distribution
- Displacement of plasma protein bound drug is seldom clinically important
- Only transient increase in free [drug] due to increase in elimination
- Problem where displacement and a reduction in elimination occur simultaneously
- Phenylbutazone displaces warfarin from albumin and inhibits metabolism of warfarin to increase bleeding
- Salicylates displace methotrexate from albumin and reduce its secretion into the nephron by competing for the anion secretory carrier
- Antiarrhythmics (quinidine, verapamil, amiodarone) displace digoxin from tissue-binding sites and reduce its renal excretion to cause severe arrhythmias through digoxin toxicity
Metabolism
Drug Interactions: Metabolism
- Drugs can either inhibit or induce drug-metabolising enzymes
- Enzyme induction
- Over 200 drugs can cause enzyme induction
- Eg rifampicin given for 3 days reduces effectiveness of warfarin as an anticoagulant


Drug Interactions: Metabolism

Drug Interactions: Metabolism
Prodrugs

Drug Interactions: Metabolism
Toxic metabolites


Drug Interactions: Metabolism
- Nearly always due to interaction at Phase I enzymes, rather than Phase II
- Phase I commonly due to interaction at cytochrome P450 enzymes – some of which are genetically absent

Drug Interactions: Metabolism
Phase I Drug Oxidation
a microsomal mixed function oxidation system

Drug Interactions: Metabolism
- Cytochrome P450 Nomenclature
- 12 families of enzymes of which 3 are involved in drug metabolism (CYP1, CYP2, CYP3)
- Each family has ~5 subfamilies (A, B, C, D, E)
- Individual isoenzymes are identified by a number (eg. CYP3A4, CYP2D6)
- Individual isoenzymes are responsible for specific metabolic steps for particular drugs
- codeine to morphine CYP2D6
- tamoxifen to desmethyltamoxifen CYP3A4
- tamoxifen to 4-hydroxytamoxifen CYP2D6

Drug Interactions: Metabolism
- CYP2Cs
- Major substrates include some nonsteroidal anti-inflammatory drugs, warfarin, phenytoin, PPIs
- Dramatic interracial polymorphism e.g. CYP2C19
- CYP2C19 activity is genetically determined, and its genetic polymorphism shows marked interracial difference.
- The incidence of the poor metaboliser phenotype is markedly higher in Asian populations (13–23%) than in white populations (2–5%) (de Morais et al., 1994)

Drug Interactions: Metabolism
- See http://medicine.iupui.edu/flockhart/
- Many, constantly changing
- Need to be aware of inhibitors, inducers and substrates and how to interpret a situation of multiple drugs
- Drug interactions (at least metabolic interactions) can be predicted based on knowledge of the characteristics of the particular drugs involved
CYP3A

Drug Interactions: CYP3A
- Responsible for metabolism of greatest number of drugs:
- Not polymorphic but activity can vary > 50 fold
- Most calcium channel blockers
- Most benzodiazepines
- Most HIV protease inhibitors
- Most HMG-CoA-reductase inhibitors
- Most non-sedating antihistamines eg terfenadine
- Antiarrhythmics eg quinidine
- Immune modulators eg. Cyclosporine
- Present in GI tract and liver
Drug Interactions: CYP3A
CYP3A Inhibitors

Common inducers include:
- Broccoli
- Brussels sprouts
- Char-grilled meat
- Chronic alcohol use
- Cigarette smoke
Drug Interactions: CYP3A
CYP3A Inducers

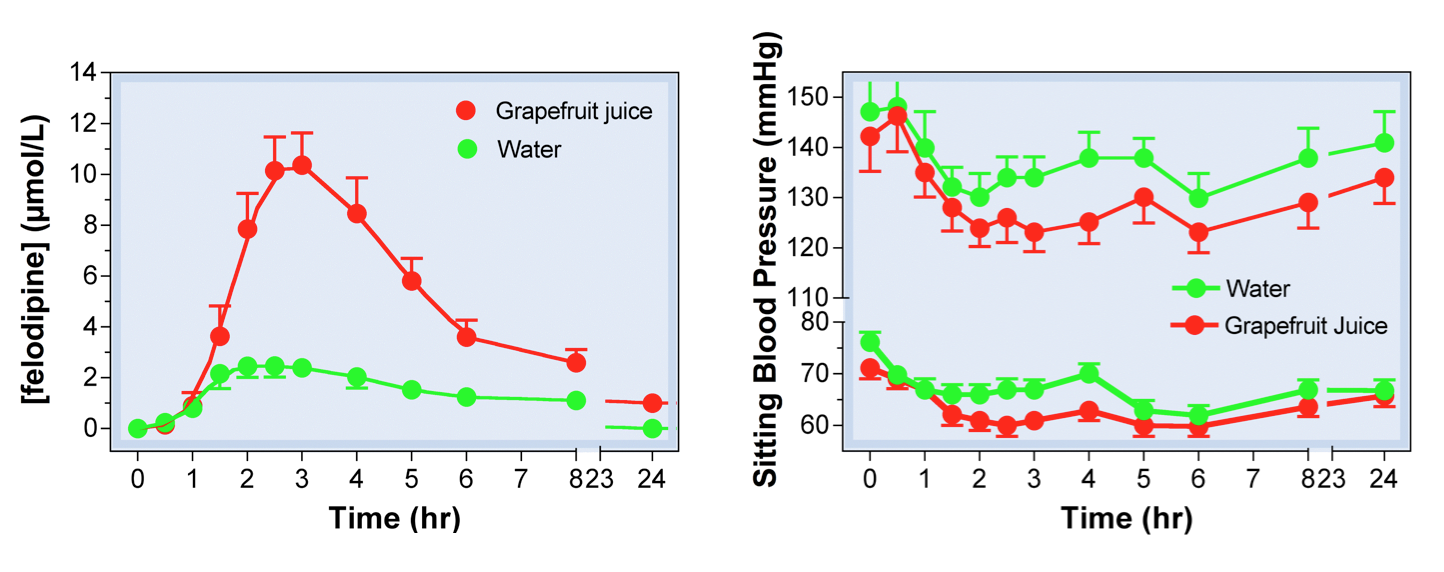
Drug Interactions: Grapefruit Juice
- Grapefruit juice inhibits CYP3A4
- Present in the GUT wall leads to drug metabolism during absorption (it will normally reduce the levels of drug that reach the systemic circulation)
- Leads to an increase in plasma concentration (Cp) of susceptible drugs
- Those affected
- Mainly metabolised by CYP3A4
- Examples
- Calcium channel blockers and statins
Drug Interactions: Grapefruit Juice
Effects of grapefruit juice on felodipine pharmacokinetics and pharmacodynamics
CYP2D6

Drug Interactions: CYP2D6
- Absent in 7% of Caucasians,1–2% non-Caucasians
- Hyperactive in up to 30% of East Africans
- Catalyzes primary metabolism of:
- Codeine
- Many β-blockers
- Many tricyclic antidepressants
- Inhibited by:
- Fluoxetine
- Haloperidol
- Paroxetine
- Quinidine


Abrupt smoking cessation can affect the metabolism of drugs
- Smoking induces the activity of human CYP1A2 and CYP2B6.
- These enzymes metabolise clozapine, olanzapine and methadone.
- Decreased CYP1A2 activity after smoking cessation increases the risk of adverse drug reactions, with reports of increased toxicity from clozapine and olanzapine.
- Replacement therapy does not influence CYP1A2 activity (chemicals in smoke involved).
CYP1A2 activity is significantly higher in heavy smokers (more than 20 cigarettes/day) than in non- smokers. This is likely to be clinically relevant for some drugs which have a narrow therapeutic index and are metabolised by CYP1A2 (Australian prescriber June 2013)
Excretion

Drug Interactions: Excretion
- One drug can affect the renal excretion of another by:
- Inhibition of tubular secretion
- Altered protein binding and filtration
- Altering urine flow or urine pH

Drug Interactions: Excretion
- Renal Excretion
- Clearance of some drugs is directly related to GFR
- digoxin, methotrexate, gentamicin
- Inhibiting tubular secretion
- See table
- Clearance of some drugs is directly related to GFR
Drug excretion 1

Drug Interactions: Excretion
- Diuretics and drug excretion:
- Diuretics tend to increase the excretion of other drugs
- Lithium is an exception since it gets treated like Na+. Initially Na+ is lost when diuretics are given but within a few days there is a compensatory Na+ (and Lithium) retention in proximal tubule.

Drug Interactions: Stepwise Approach
- 1. Take a good medication history
- 2. Remember high risk patients and drugs
- Any patient taking >2 medications
- Anticonvulsants, antibiotics, digoxin, warfarin, amiodarone, etc
- 3. Check pocket reference
- 4. Consult pharmacists/drug info specialists
- 5. Check up-to-date computer program, e.g.
- http://medicine.iupui.edu/flockhart/
- www.drug-interactions.com
- www.clinicalpharmacologyonhand.com/marketing/about_cpoh.html (available on PDA)
- www.epocrates.com (available on PDA)
- eMIMS (available on PDA)
- one
- tedft
- tyyjty
- ghhj