A/Prof. Ken Rodgers School of Life Sciences
Contents
References
- Rang HP, Dale MM, Ritter JM, Flower RJ, Henderson, G (2016) Pharmacology, 8th Edition, Churchill Livingstone, Sydney.
- How drugs act: general principles– Section 1, part 2
What are Agonists and Antagonists?
What is an agonist?
- Drug, hormone, toxin, autacoid or neurotransmitter that elicits a biological effect when it interacts with receptors – bethanechol (used for urinary retention) combines with muscarinic ACh receptor
- Bethanecholmimics action of ACh (the neurotransmitter at these receptors)
- Magnitude of signal depends on number of receptors occupied and/or rate of formation of drug-receptor complexes
- Signal amplified by intracellular mechanism
What is an antagonist?
A drug which interacts with a receptor, does not elicit a biological effect and blocks or reverses the effect of an agonist
Agonist v antagonist

Affinity vs efficacy
Other definitions 1
- What is affinity?
- Relative tendency of a drug to combine with its receptor
- What is intrinsic activity or efficacy?
- Capacity of a drug to produce a pharmacological effect after binding to its receptor ie the maximal possible effect than can be produced by the drug (Emax)
- Agonists possess?
- Affinity and intrinsic activity
- Antagonists possess?
- Affinity but lack intrinsic activity

Affinity
- The response of the cell is a product of affinity and efficacy (intrinsic activity)
- Drug A fits the receptor better than Drug B
- Drug A has a greater affinity for this receptor than Drug B

Intrinsic activity/efficacy
- The response of the cell is due to affinity and intrinsic activity
- Drug C has a greater intrinsic activity at this receptor than Drug A
Partial agonists and spare receptors

Other definitions 2
- Partial agonist
- Compound which interacts with a receptor but produces less than the maximum effect – less intrinsic activity or efficacy. Even with 100% receptor binding it does not produce a maximal response.
- Eg. buprenorphine (partial agonist at µ opioid receptor) produces less analgesia than morphine (full agonist)
- Spare receptors
- Implied, when the maximum effect is produced with less than 100% receptor occupancy. Requires functional as well as binding studies.
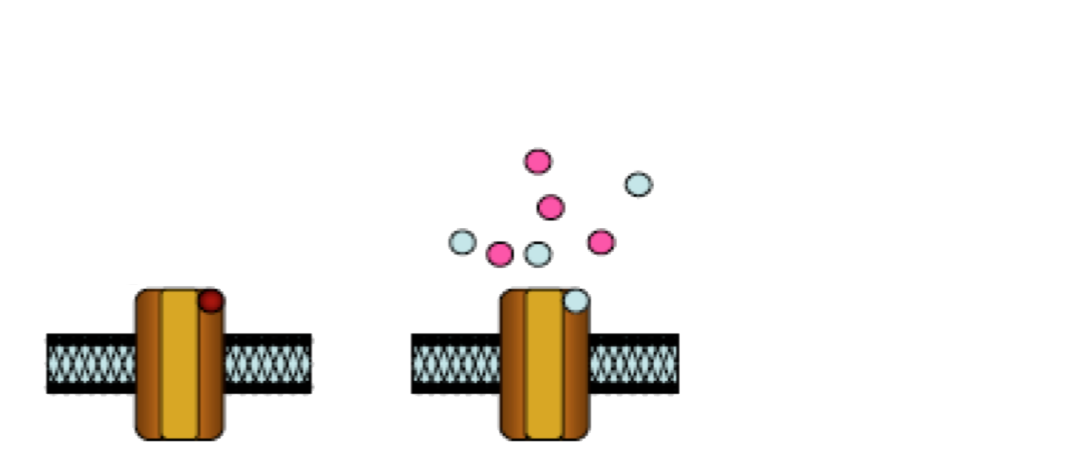
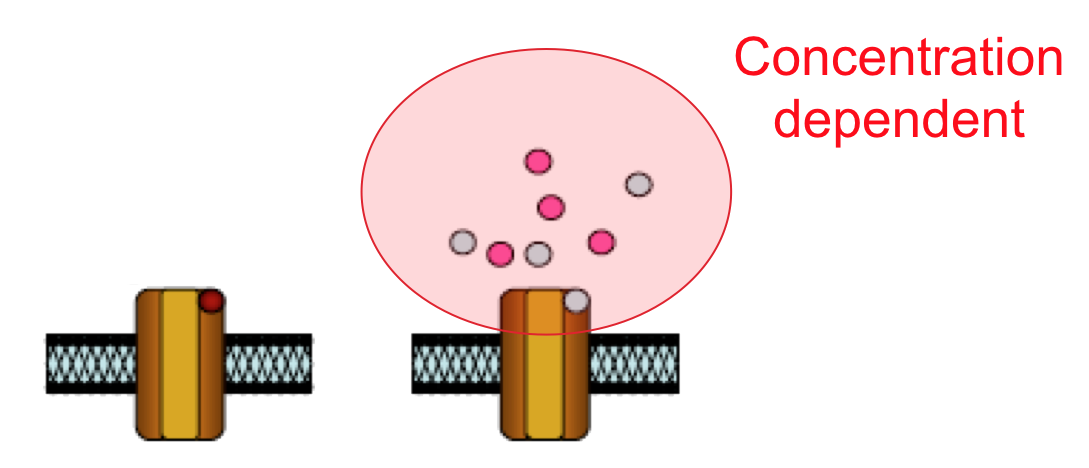
Biased agonism
Two agonists bind at the same site on the receptor yet the red agonist is better at evoking response 1 and the green agonist is better at evoking response 2.

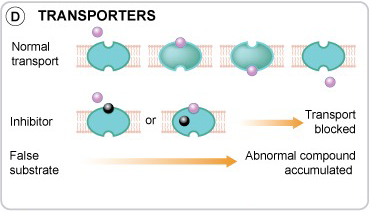
Types of receptor antagonism
Type of receptor antagonism
- Competitive
- Compete for the binding site
- Reversible
- Irreversible
- Compete for the binding site
- Non-competitive (Allosteric modulation)
- Bind elsewhere eg. Ion channel blockers

Types of antagonism 1
- Reversible competitive antagonist
- Agonist competes with antagonist for same receptor
- [antagonist] progressively inhibits the agonist response
- Parallel shift of dose response (DR)-curve to the right and ED50 is altered
- But blockade CAN be reversed by a higher dose of agonist
- ie the same Emax is reached
- eg atropine (muscarinic receptor antagonist)

Types of antagonism 1
- Reversible competitive antagonist
- Agonist competes with antagonist for same receptor.
- Parallel shift of DR-curve to the right and ED50 is altered.
- But blockade CAN be reversed by a higher dose of agonist.
- The same Emax is reached
- eg atropine (muscarinic receptor antagonist)
Types of antagonism 3
- Irreversible competitive antagonist
- Antagonist binds at same site.
- Antagonist dissociates slowly, or not at all, from the receptors – irreversible bond (eg covalent bond)
- No change in the antagonist occupancy takes place when the agonist is applied.
- Thus blockade CANNOT be reversed by higher dose of agonist
- Prevent agonists from producing any effect – Emax is but the agonist acts normally at the unoccupied receptors
- Thus no shift in DR-Curve ie. no change in ED50 for agonist
- eg. methysergide (5-HT receptor antagonist) used in Rx of migraine
- eg. α-neurotoxins from snake venom (nicotinic receptor antagonist)
Types of antagonism 4

Types of antagonism 3
- Irreversible competitive antagonist
- Antagonist dissociates slowly, or not at all, from the receptors – irreversible bond (eg covalent bond)
- No change in the antagonist occupancy takes place when the agonist is applied
- Thus blockade CANNOT be reversed by higher dose of agonist
- Prevent agonists from producing any effect – Emax is but the agonist acts normally at the unoccupied receptors
- Thus no shift in DR-Curve ie. no change in ED50 for agonist
- eg. methysergide (5-HT receptor antagonist) used in Rx of migraine
- eg. α-neurotoxins from snake venom (nicotinic receptor antagonist)
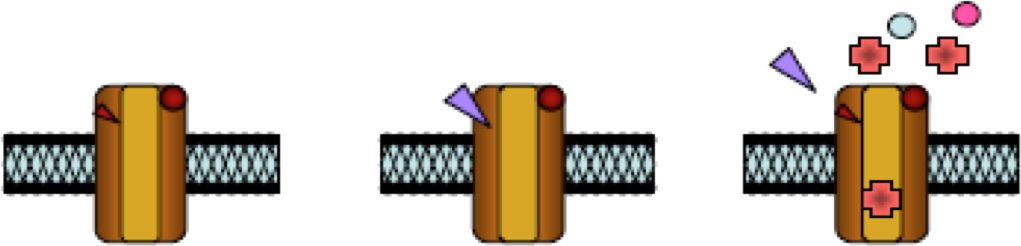
Types of antagonism 5
- Non-competitive antagonism or allosteric modulation of receptor function
- Bind at a site close to but distinct from the agonist receptor site
- Only have an effect on receptors that are activated
- May be an ion channel or G-protein linked to the receptor ie block in receptor-effector linkage since it acts at different site
- Eg. suxamethonium(depolarising muscle relaxant)desensitises nicotinic receptor ion channel
- Eg. calcium antagonists (eg verapamil and nifedipine) non-specific block of contractions by other drugs
Types of antagonism 6


Types of antagonism 7
- Physiological Antagonism
- Blockade of an effect due to production of an effect in the opposite direction (acts via separate cells or separate physiological systems or opposing receptors)
- Eg. In gut – ACh contraction mediated through muscarinic receptor antagonised by noradrenaline (Nad) relaxation mediated through beta receptor
- Weak partial agonists can also seem to be like competitive antagonists
- If receptors are constitutively active the addition of a weak agonist can actually decrease receptor activation these are known as ‘inverse agonists’
Desensitization and tachyphylaxis
Desensitization and tachyphylaxis 1
- Synonymous terms – a drug effect which gradually diminishes over a few seconds to minutes
- Causes
- Change in receptors
- Receptor resulting in tight binding of agonist without opening of ion channel
- Exhaustion of mediators
- Depletion of neurotransmitters or second messengers
- Change in receptors
Tolerance (days or weeks to develop)
- Causes
- Increased metabolic degradation
- Induction of metabolic enzymes eg barbiturates/ethanol in liver
- Physiological adaptation
- Eg. side effects (nausea, sleepiness) sometimes tend to subside
- Translocation of receptors (hours)
- Receptors may be internalised by endocytosis and degraded in lysosomes eg. gonadotrophin-releasing hormone inhibits gonadotrophin release by continuous receptor stimulation (usually pulsatile) used in prostatic cancer.
- Increased metabolic degradation
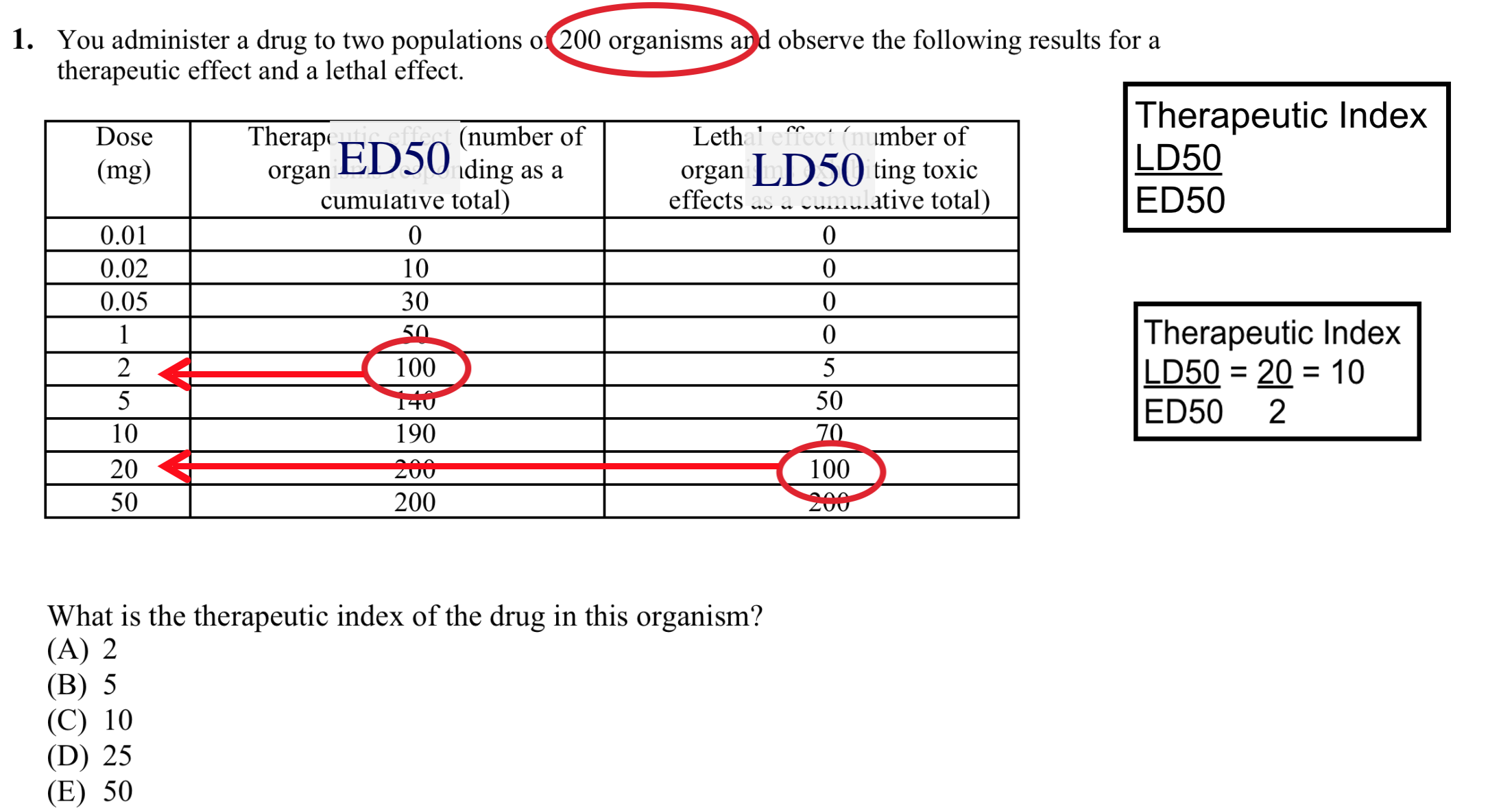
Drug Toxicity

Drug toxicity 1
- “All things are poisons, nothing is without poisonous qualities. It is only the dose which makes a thing a poison”
Paraphrased from Paracelsus (1493-1541)
- Potency provides little information about the dose of drug at which toxic effects manifest themselves
- Determined from the LD50 (median lethal dose)
- Dose of drug that is lethal to 50% of subjects

Drug Toxicity 2
- Thus therapeutic index (LD50/ED50) gives an idea of the relative margin of safety of a drug
- Greater this ratio the safer the drug
- Must be >1.0 to be therapeutic agent, <2.0 typically see toxicity at therapeutic dose
- Therapeutic index:
- Digoxin (Rx heart failure)= 1.5-2.0, vs.
- Penicillin (antibiotic) >100 (non-allergic patients)

Drug Toxicity 2
- Thus therapeutic index (LD50/ED50) gives an idea of the relative margin of safety of a drug
- Greater this ratio the safer the drug and must be >1.0 to be therapeutic agent, <2.0 typically see toxicity at therapeutic dose
- Therapeutic index:
- Digoxin (Rx heart failure) = 1.5-2.0, vs.
- Penicillin (antibiotic) >100 (non-allergic patients)
- Depends on therapeutic use – certain situations (eg. anaesthesia) may require higher dose of drugs than other situations (eg. sedation, sleep)
- Since the ED50 goes up while the LD50 remains unchanged, the therapeutic index goes down (ie greater risk of toxicity)
Therapeutic Index
Drug targets: receptors

Drug targets: enzymes

Drug targets: enzymes